16 Dec 2024
This article has been reviewed by Lester Morse, Director of Rehabs UK, who has over 30 years of experience helping individuals overcome various forms of addiction. Rehabs UK is a leading authority in addiction treatment and recovery and offers a range of connected services and support, including detox and rehabilitation programmes and therapy.
Opioids are commonly used as both prescribed medications for managing severe pain and as substances of abuse across the world. They include prescription medications such as Tramadol and Fentanyl, which play a significant role in modern medicine, and class-A drugs like Heroin.
Opioids can relieve some chronic pain conditions as well as post-surgical pain, but their use isn’t without risks and they are also known for their potential to cause addiction and respiratory depression. Emerging evidence also suggests opioids can also have a detrimental effect on the liver.
In certain cases, liver damage is linked to the opioids themselves, while in others, it is due to the presence of additional substances like paracetamol in combination drugs.
This article will look at how opioids can affect liver health, highlighting specific drugs and the broader impacts of opioid addiction on liver function.
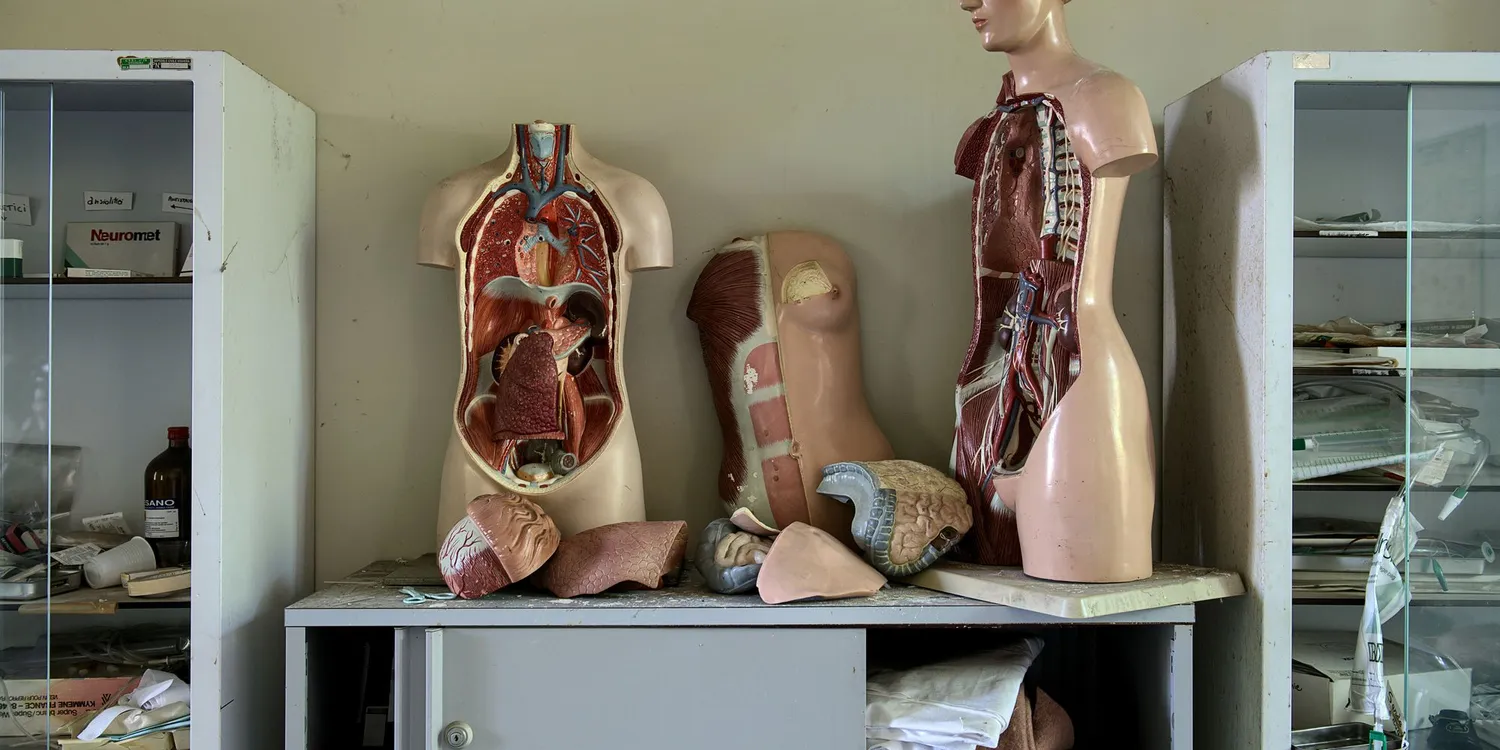
The importance of your liver
One of the most vital organs in your body is the liver. It’s the body's natural detoxifier, metabolising drugs, filtering toxins from the blood and aiding in digestion by producing bile and proteins necessary for blood clotting. The organ also has a crucial role in regulating the body’s cholesterol levels and stores nutrients such as iron and vitamin A.
The liver filters more than a litre of blood every minute, which is about 22 gallons of blood per hour and more than 250 gallons of blood in a 24-hour time period.
Due to the importance of the liver's role in detoxification and drug metabolism, it is particularly vulnerable to damage from certain substances including opioids.
When the liver is compromised, its ability to perform these functions is diminished, which can lead to a range of health problems.
How different opioids can affect your liver
There are various effects that opioids can have on the liver, this all depends on the specific drug, duration of use, dosage, and presence of additional substances.
Here’s a breakdown of how some commonly used opioids can impact the liver;
Tramadol
The popular prescription painkiller, Tramadol, is often used for moderate to severe pain. It is generally considered to be one of the safer opioids for the liver, however, prolonged use or high doses of Tramadol can lead to liver enzyme elevations which indicates stress on the liver.
A 2015 study found that there was a risk of increased liver and kidney damage due to the long-term use of tramadol. Other research has shown that taking tramadol with acetaminophen (paracetamol) may cause complications, including acute liver failure.
In some rare cases, Tramadol use has been connected with liver damage, particularly with other liver-affecting substances such as alcohol or over-the-counter pain relievers.
Co-codamol
Co-codamol is a combination of codeine and paracetamol. While codeine itself can be harsh on the liver, the real concern with Co-codamol often lies in its paracetamol content. If paracetamol is used in high doses or quantities exceeding the recommended dose, it is known to cause acute liver failure.
Co-codamol used regularly can lead to an accumulation of paracetamol in the liver, increasing the risk of liver toxicity.
How Can I Protect My Liver When Taking Co-Codamol?
- Protecting your liver while using Co-codamol involves careful adherence to guidelines and a proactive approach to managing potential risks. Here are some key steps:
- Follow the Recommended Dosage Always take Co-codamol as prescribed by your healthcare provider or as indicated on the packaging. Avoid exceeding the recommended dose, even if your pain persists, as this increases the risk of paracetamol accumulation and liver toxicity.
- Limit Alcohol Consumption Alcohol is processed by the liver, and combining it with Co-codamol can significantly increase the strain on this vital organ. Avoid drinking alcohol while taking Co-codamol to reduce the risk of liver damage.
- Avoid Other Medications Containing Paracetamol Many over-the-counter medications, such as cold and flu remedies, also contain paracetamol. Taking these alongside Co-codamol can unintentionally lead to an overdose of paracetamol. Always read labels carefully and consult your pharmacist or doctor if you are unsure.
- Monitor Duration of Use Co-codamol is intended for short-term use. Regular or prolonged use increases the risk of liver toxicity and dependency. If you need pain relief for an extended period, discuss alternative treatments or management plans with your healthcare provider.
- Stay Hydrated and Maintain a Balanced Diet Keeping your liver healthy involves overall good health practices, including staying hydrated and eating a balanced diet rich in antioxidants, vitamins, and minerals to support liver function.
- Be Aware of Early Signs of Liver Issues Symptoms such as nausea, vomiting, abdominal pain, yellowing of the skin or eyes (jaundice), or unusual fatigue could indicate liver problems. If you notice these signs, stop taking Co-codamol and seek immediate medical attention.
- Consult Your Doctor Regularly If you have underlying health conditions such as liver disease or are taking other medications, discuss these with your doctor before starting Co-codamol. They may recommend blood tests or other monitoring to ensure your liver remains healthy
Subutex
Subutex otherwise known as buprenorphine, is often used to replace therapy to help individuals recover from opioid addiction. Many people consider the drug much safer than methadone although as with many drugs long-term use has been linked to elevated liver enzymes in some patients which can indicate liver stress or damage.
Lester Morse, Director of Rehabs UK states: “in my opinion Subutex is less harmful than methadone, however it is still masking the problem of the individual’s addiction.”
Some studies suggest that liver toxicity is more common in patients with pre-existing liver conditions, making it essential to monitor liver function during treatment.
Fentanyl
Fentanyl is a powerful synthetic opioid, significantly stronger than morphine. The drug is commonly used in severe pain management, particularly in cancer patients. Fentanyl isn't generally considered hepatoxic. However, it is usually administered in a controlled medical setting.
There is a huge risk primarily when fentanyl is illicitly manufactured. This is where batches may contain unknown impurities or addictive that can damage the liver. Fentanyl overdoses are increasingly common with illicit use, a large population of the USA and Canada has been affected by this fentanyl epidemic.
Almost 500,000 Americans fatally overdosed on opioids, like codeine, from 1999 to 2019. Opioids like codeine share common properties that contribute not only to their addictive potential but also to their effects on liver health. These substances are metabolised in the liver, where prolonged or excessive use can lead to hepatotoxicity, impairing liver function and potentially causing long-term damage. This connection highlights the importance of understanding the interplay between opioid use and liver health to mitigate risks and develop safer pain management strategies.
The indirect impact of opioid addiction on your liver
Opioid addiction can have several indirect effects due to lifestyle changes and co-occurring behaviours rather than just directly through the drugs themselves.
Diet
As with a lot of drug addictions, usage can lead to poor dietary habits. It could decrease appetite or make the individual prioritise the drug over nutrition. Due to this, the body lacks essential nutrients which can compromise liver function and, in turn, can lead to fatty liver disease or other metabolic issues. If your liver is healthy, a well-balanced diet can reduce your risk of developing some types of liver disease in the future.
Alcohol abuse
Opioid addiction can commonly be paired with alcohol abuse, which compounds the risk of liver damage hugely. Alcohol is a known hepatotoxin; mixing it with opioids can accelerate liver deterioration, and it even has the potential to lead to cirrhosis or liver failure.
Of the 98,457 liver disease deaths among people aged 12 and older in 2022, 46.0% involved alcohol. Among males, 60,412 liver disease deaths occurred, with 48.6% involving alcohol.
Physical activity
Physical inactivity reduces the liver's ability to process fats, which then leads to a build-up in the liver cells, which increases the risk of non-alcoholic fatty liver disease. Opioid use can lead to a sedentary lifestyle and therefore contributes to obesity, fatty liver disease and other metabolic disorders.
Not only is exercise good for your heart, mental health, and energy levels, but it also helps reduce your risk of developing chronic liver disease. The NHS recommends doing at least 2½ hours of moderate cardio each week and strengthening exercises twice every week.
Signs of liver damage
Liver damage can manifest in various ways, some of which may be exacerbated by opioid use:
Jaundice: This occurs when the liver cannot effectively filter out bilirubin, a by-product of red blood cells. The result is yellowing of the skin and eyes.
Abdominal pain and swelling: This can indicate liver inflammation or fluid accumulation.
Chronic fatigue and weakness: These symptoms are often related to the liver's reduced ability to detoxify the body.
Dark urine and pale stools: These may signal bile duct blockages or liver dysfunction.
If you notice any of these symptoms, it's crucial to seek medical attention promptly.
What can I do when I have liver damage?
If you've been diagnosed with liver damage, early intervention is key to preventing further deterioration. This can include:
Detoxification: Removing harmful substances from your body under medical supervision.
Medication adjustments: Switching to less hepatotoxic pain management options.
Lifestyle changes: Improving diet, increasing physical activity and reducing alcohol intake.
Proper rehabilitation and medical care can help restore liver function, especially if the damage is caught early.
Get in touch today
If you or a loved one is struggling with opioid use and concerned about liver health, reaching out to a specialist is the first step. At Rehabs UK, we offer comprehensive treatment programmes tailored to each individual's needs. Contact our fully trained Treatment advisors who will be able to answer any questions and point you in the right direction going forward once they have conducted a free assessment.